Take time out of your busy day and make a Donation to an amazing cause. Shed some light on Heart Awareness
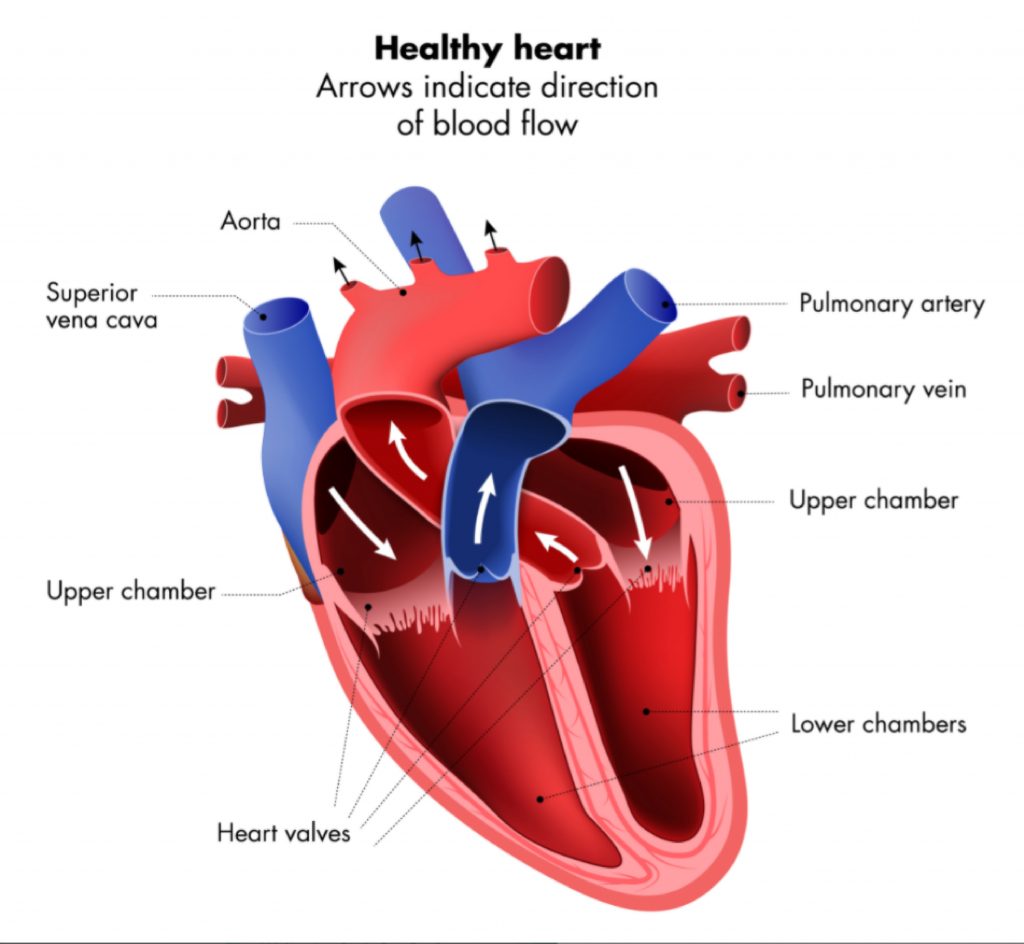
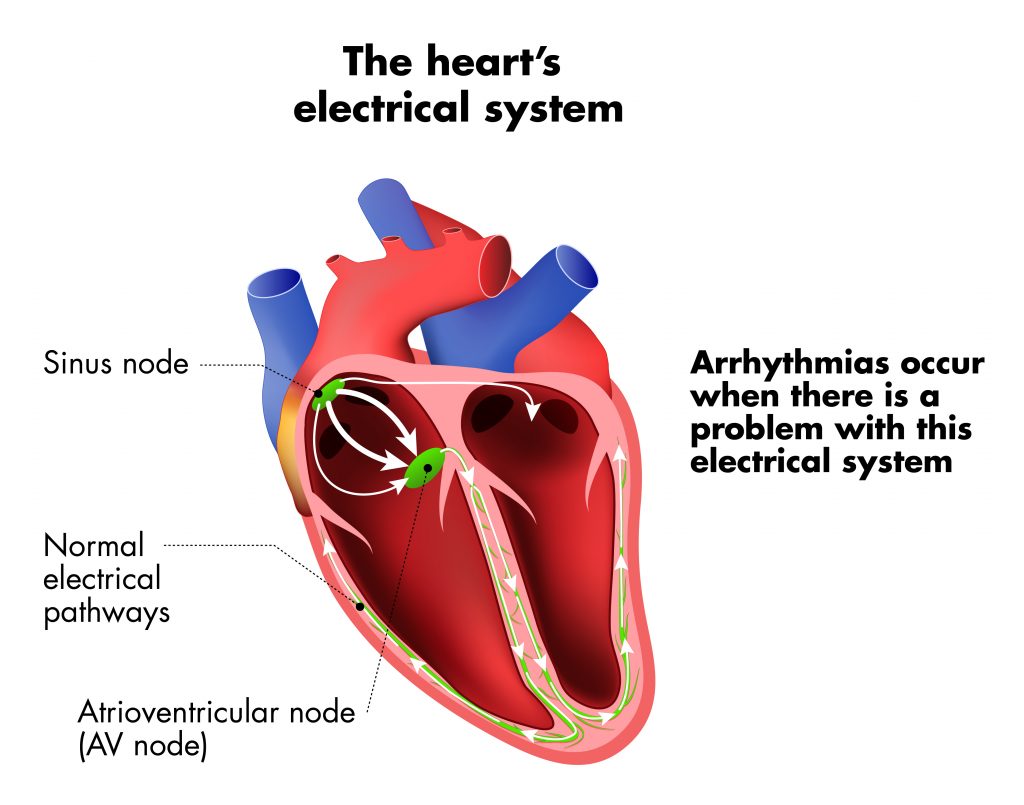
A heart arrhythmia is a problem with the rhythm of the heartbeat. Arrhythmias happen due to problems with the electrical system that controls the pumping of the heart. During an arrhythmia, abnormal electrical signals cause the heart to beat too quickly, too slowly, or irregularly. Some arrhythmias only occur briefly, but when an arrhythmia lasts longer it can cause the heart to pump less efficiently.
Not all arrhythmias are dangerous, and some have no effect on your ability to lead a normal life. Others can be more serious, and some need urgent treatment. With proper treatment and management, most people with arrhythmias can lead a full and enjoyable life.
There are two main categories of arrhythmias. These are based on how fast the person’s heart beats whilst resting:

This is where the heart beats faster than normal, at a resting heart rate of more than 100 beats per minute.

This is where the heart beats more slowly than normal, with a resting heart rate of less than 60 beats per minute.
Arrhythmias can be caused by a number of conditions including:
If you have a paroxysmal arrhythmia, try to work out what may cause it so you can avoid these triggers. If your triggers include medicines or exercise, speak to your doctor. They can suggest alternative medicines or activities that may be more suitable for you.
Heart arrhythmias don’t always need to be treated. They may only need treatment if the arrhythmia is causing health problems or symptoms. Although some arrhythmias are serious, with the right medical treatment and positive lifestyle changes people with arrhythmias can still have a good quality of life.
Treatments for arrhythmias vary depending upon their cause and how the arrhythmia impacts you. Options may include medicine, surgery, medical procedures and devices. When considering which treatment is right for you, it is a good idea to get opinions from more than one health professional, eg from a cardiologist and a surgeon.
These help maintain or restore a normal heart rhythm. There are several different types of anti-arrhythmic medicines, and they can either bring the heart back to a normal rhythm, or can be used to prevent an arrhythmia. Types of anti-arrhythmic medicines include beta blockers and calcium channel blockers (see below), as well as sodium channel blockers and medicines that block potassium channels in the heart.
Some common anti-arrhythmic medicines include:
These work by slowing your heart rate and reducing blood pressure. They do this by blocking the effects of the hormone adrenaline. By slowing the heart rate they can improve symptoms of arrhythmias, including palpitations and fatigue. This can help you feel better and get back to your normal daily activities.
Types of beta blockers include:
Possible side effects include:
If you experience side effects, speak to your doctor about them.
Some beta blockers can make the symptoms of asthma worse. If you have asthma, make sure it is well controlled, and let your doctor know if you become wheezy or short of breath. Beta blockers can sometimes hide the signs of low glucose levels, so if you have diabetes you may need to check your blood sugar more often when taking beta blockers. You should not stop taking beta blockers suddenly, since this can increase your risk of heart attack or other heart problems. Speak to your doctor before you stop taking a beta blocker.
These can be used to slow a fast heart rate or the speed at which the heart’s electrical signals travel. They work by stopping calcium from entering the cells of the arteries and the heart. Calcium causes the arteries and heart to contract harder. Blocking calcium has an effect on the sinus and atrioventricular nodes which control the heartbeat, and so can help to control arrhythmias. These medicines can help decrease your symptoms and improve your quality of life.
Types of calcium channel blockers include:
Possible side effects can include:
If you experience side effects, speak to your doctor about them. Seek medical treatment urgently if you experience chest pain, dizziness, shortness of breath, fainting or collapse while taking calcium channel blockers. You should not stop taking calcium channel blockers suddenly. Speak to your doctor before you stop taking a calcium channel blocker.
This can also be used to treat a fast heart rate. It helps to slow the heart rate and improve the ability of the lower chambers of the heart to fill with blood. It works by changing the levels of some minerals (including sodium and calcium) in the cells, which can help the heart to beat with more force. It can help to manage symptoms of arrhythmias that have not been controlled by other treatments.
Possible side effects can include:
See your doctor as soon as possible if you have more than 2 of the side effects listed above, or if you have a fast heart rate, shortness of breath, feel dizzy and are sweating. Your doctor may have you do regular blood tests to check the levels of digoxin in your body, as well as to check your kidney function. This is to make sure the medicine is safe for you. You should not stop taking digoxin suddenly. Speak to your doctor before you stop taking digoxin.
Can help prevent blood clots from forming, and may be prescribed if your arrhythmia increases the risk of having a stroke. They work by interrupting the processes that cause blood clots to form. They are important because they can help to reduce your risk of having a stroke or heart attack if you have a high chance of developing blood clots.
Types of anticoagulant medicine include:
The main side effect of anticoagulants is that you can bleed more easily than usual. This can cause symptoms including:
For most people who need anticoagulants, their benefits outweigh the risks. Your doctor can help you to weigh up the risks and benefits of these medicines. If you are taking warfarin, you will need to have regular blood tests to check that it is working safely for you. You will also need to keep an eye on your diet, since some foods and drinks can affect how this medicine works. If you are taking other kinds of anticoagulant medicine, you may need to have a blood test every 6 to 12 months, to check that your kidneys are working properly.
![]() This is where a long, flexible tube is inserted to modify the area inside the heart that is causing the abnormal rhythm.
This is where a long, flexible tube is inserted to modify the area inside the heart that is causing the abnormal rhythm.
The tube is used to direct heat (radiofrequency ablation) or cold (cryoablation) energy to the tissues that are creating the abnormal signals. This energy is used to modify these tissues. Some of these procedures can take 4 hours or more. You may be able to go home on the same day, or you may need to stay in hospital overnight. Most people can return to their normal activities within a few days, but you should avoid strenuous activities or lifting heavy items for a few days.
Risks of ablation can include: infection after surgery, damage to blood vessels or heart valves, a new or worsening arrhythmia
(in some rare cases needing a pacemaker), blood clots, stroke or heart attack. Your doctor will discuss the risks and benefits of this treatment with you. Although there are a number of possible risks, the procedure is generally considered low risk, and can be done with an overnight stay or as a day procedure.
![]() This is a type of ablation that targets and modifies the AV node, a nerve that transmits electrical signals from the upper chambers of the heart to the lower chambers of the heart. It is used to treat atrial fibrillation when medicine has not been enough to control the condition. This procedure permanently stops the electrical connection between the upper and lower chambers of the heart, so you will need to have a pacemaker implanted to regulate your heartbeat before having an AV node ablation. This option is used when other treatment methods have not been successful. It helps the heart to beat in a controlled manner, helping you to feel better. Risks of the procedure are similar to those for catheter ablation.
This is a type of ablation that targets and modifies the AV node, a nerve that transmits electrical signals from the upper chambers of the heart to the lower chambers of the heart. It is used to treat atrial fibrillation when medicine has not been enough to control the condition. This procedure permanently stops the electrical connection between the upper and lower chambers of the heart, so you will need to have a pacemaker implanted to regulate your heartbeat before having an AV node ablation. This option is used when other treatment methods have not been successful. It helps the heart to beat in a controlled manner, helping you to feel better. Risks of the procedure are similar to those for catheter ablation.
![]() This procedure delivers a shock to the heart to help it get back to a normal rhythm. Electrode pads are placed on the chest, and medicine is given through a vein to put you to sleep during the procedure. The electrodes are connected to a cardioversion machine (defibrillator) via wires. This machine checks the rhythm of your heart and delivers shocks to the heart to restore a normal rhythm. Once you are asleep, the procedure usually only takes a few minutes. Most people will stay at the hospital for a few hours, and go home later that day.
This procedure delivers a shock to the heart to help it get back to a normal rhythm. Electrode pads are placed on the chest, and medicine is given through a vein to put you to sleep during the procedure. The electrodes are connected to a cardioversion machine (defibrillator) via wires. This machine checks the rhythm of your heart and delivers shocks to the heart to restore a normal rhythm. Once you are asleep, the procedure usually only takes a few minutes. Most people will stay at the hospital for a few hours, and go home later that day.
Risks of the procedure include: developing another abnormal heart rhythm, dislodging existing blood clots, or skin damage where the electrodes are placed. These risks are uncommon, and your doctor will discuss the risks and benefits of this treatment with you. For most people, the procedure quickly restores a normal heartbeat, allowing you to get back to your usual activities. Long term medication may also be needed to help the heart to continue beating normally.
![]() Surgical ablation can take the form of a maze operation. This is similar to ablation, but produces a ‘maze’ of small scars in the upper chambers of the heart. This scar tissue does not carry electrical signals, so it stops the abnormal electrical signals that cause AF from travelling within the heart. It is usually done when the person also needs heart surgery for other reasons, such as a heart valve repair. The procedure takes around 3 hours, and you can expect to stay in hospital for around 7 to 10 days. Most people are able to return to their usual activities within around 3 months.
Surgical ablation can take the form of a maze operation. This is similar to ablation, but produces a ‘maze’ of small scars in the upper chambers of the heart. This scar tissue does not carry electrical signals, so it stops the abnormal electrical signals that cause AF from travelling within the heart. It is usually done when the person also needs heart surgery for other reasons, such as a heart valve repair. The procedure takes around 3 hours, and you can expect to stay in hospital for around 7 to 10 days. Most people are able to return to their usual activities within around 3 months.
Risks of the procedure are rare, but include: infection following surgery, bleeding, blood clots which can lead to a stroke or heart attack, kidney failure, or other abnormal heart rhythms. Your doctor will discuss the risks and benefits of this treatment with you. Although there are some risks, this procedure can improve symptoms and quality of life.
![]() This uses a small electrical current to get the heart’s rhythm back to normal during a cardiac arrest caused by a life threatening arrhythmia. It is a portable device that checks the rhythm of the heart, prompting the user to deliver a shock if needed. An AED is used to defibrillate the patient and restore the heart’s rhythm. A person who has had a cardiac arrest and had an AED used will need to go to hospital for further care and treatment.
This uses a small electrical current to get the heart’s rhythm back to normal during a cardiac arrest caused by a life threatening arrhythmia. It is a portable device that checks the rhythm of the heart, prompting the user to deliver a shock if needed. An AED is used to defibrillate the patient and restore the heart’s rhythm. A person who has had a cardiac arrest and had an AED used will need to go to hospital for further care and treatment.
![]() This is a device implanted in the body that monitors the heart’s rhythm and corrects it if necessary. This may be used for when medicines have not worked. ICDs can help treat arrhythmias when they occur, and have the benefit of reducing risk of cardiac arrest. Surgery to implant the device usually takes one to two hours, and you will usually be able to go home the next day. It may take a few weeks of recovery before you are able to return to your usual daily activities.
This is a device implanted in the body that monitors the heart’s rhythm and corrects it if necessary. This may be used for when medicines have not worked. ICDs can help treat arrhythmias when they occur, and have the benefit of reducing risk of cardiac arrest. Surgery to implant the device usually takes one to two hours, and you will usually be able to go home the next day. It may take a few weeks of recovery before you are able to return to your usual daily activities.
Risks associated with having an ICD include infection when having the device surgically implanted, damage to blood vessels caused by the ICD leads, blood leaking through the heart valve where the ICD lead is placed, and lung collapse. There is also a small chance that the device may fail before it is due to be replaced, or that the ICD leads may move within the body and another surgery may be needed to put them back in place. Your doctor will discuss the risks and benefits of this treatment with you. An ICD can reduce risk of cardiac arrest and improve your quality of life.
![]() This is a device that is implanted in the body that sends electrical signals to the heart and help it keep a steady heart rhythm. A pacemaker can be implanted either on the surface of the heart or inside one of the heart’s chambers, and is a small metal device that contains electrical circuitry that controls the rate of electrical pulses delivered to the heart. The procedure to implant a pacemaker usually takes 1 to 2 hours, and you can generally go home within 1 to 2 days after surgery. You will usually be able to go back to your normal routine within 1 to 2 weeks after surgery, and reach a full recovery after a couple of months.
This is a device that is implanted in the body that sends electrical signals to the heart and help it keep a steady heart rhythm. A pacemaker can be implanted either on the surface of the heart or inside one of the heart’s chambers, and is a small metal device that contains electrical circuitry that controls the rate of electrical pulses delivered to the heart. The procedure to implant a pacemaker usually takes 1 to 2 hours, and you can generally go home within 1 to 2 days after surgery. You will usually be able to go back to your normal routine within 1 to 2 weeks after surgery, and reach a full recovery after a couple of months.
Risks of getting a pacemaker include: infection following implantation, bruising or bleeding at the site of implantation, blood clots, damage to blood vessels or nerves, bleeding between the lung and chest wall, collapsed lung, problems with the device stimulating muscles other than the heart, or problems with the device or its leads moving within the body. These risks are uncommon, and your doctor will discuss the risks and benefits of this treatment with you. A pacemaker can help improve your daily life, and allow you to get back to your usual activities.
![]() When people are not able to take anticoagulant medicines, a small device can be implanted into the heart via a catheter (narrow tube). This device is guided through the blood vessel and placed so that it seals off a part of the heart where blood clots could form. It stops blood clots from moving to other parts of the body, and so can help to prevent stroke. The procedure to implant the device usually takes around an hour, and you will need to stay in hospital overnight. You can usually go back to your usual daily activities after around a week, but should avoid strenuous activities (eg going to the gym, picking up heavy items) for two weeks.
When people are not able to take anticoagulant medicines, a small device can be implanted into the heart via a catheter (narrow tube). This device is guided through the blood vessel and placed so that it seals off a part of the heart where blood clots could form. It stops blood clots from moving to other parts of the body, and so can help to prevent stroke. The procedure to implant the device usually takes around an hour, and you will need to stay in hospital overnight. You can usually go back to your usual daily activities after around a week, but should avoid strenuous activities (eg going to the gym, picking up heavy items) for two weeks.
This device has the advantage that it does cause a risk of bleeding. So it can be an option for people who are not able to take anticoagulant medicines due to risk of bleeding.
There are some risks associated with this device. A small number of people with the device still suffer stroke, or blood clots around the device. It can also cause fluid build up in the membrane around the heart, damage to structures in the heart, bleeding, bruising, infection following the placement procedure, or the device can become dislodged. Your doctor will discuss the risks and benefits of this device with you.
![]() This is another device that can be implanted to help prevent blood clots and stroke in people who are not able to take anticoagulant medicines. It is a clip made from metal and covered with cloth that helps the AtriClip become incorporated into the heart’s tissues. The surgeon makes three small openings in the side of the chest, which they use to place the clip on the outside of the heart. The clip is used to seal off a part of the heart where blood clots could form, stopping blood clots from moving to other parts of the body, and so helping to prevent stroke. The procedure to implant the device usually takes around 30 minutes, and most people stay in hospital for around 2 days after surgery. You can usually go back to your usual daily activities after about a week, but you should not drive for 2 weeks after the procedure.
This is another device that can be implanted to help prevent blood clots and stroke in people who are not able to take anticoagulant medicines. It is a clip made from metal and covered with cloth that helps the AtriClip become incorporated into the heart’s tissues. The surgeon makes three small openings in the side of the chest, which they use to place the clip on the outside of the heart. The clip is used to seal off a part of the heart where blood clots could form, stopping blood clots from moving to other parts of the body, and so helping to prevent stroke. The procedure to implant the device usually takes around 30 minutes, and most people stay in hospital for around 2 days after surgery. You can usually go back to your usual daily activities after about a week, but you should not drive for 2 weeks after the procedure.
This device has the advantage that it does cause a risk of bleeding. So it can be an option for people who are not able to take anticoagulant medicines due to risk of bleeding.
There are some risks associated with this device. A small number of people with the device still suffer stroke, or blood clots around the device. It can also cause fluid build-up in the membrane around the heart, damage to structures in the heart